This white paper utilizes affinity mapping to chart digital patients experience expectations based on user interviews & testing across therapeutic areas.
Introduction
Over recent years, the expectations of patients and consumers in the digital world have increasingly aligned. Digital experiences now form an integral part of everyday life and are continually evolving. Consumer brands have transformed our interactions with technology through a seamless user experience (UX) across various platforms. Consequently, patients now anticipate a similar degree of ease and efficiency from other brands, including healthcare.1
Historically, until the early 2000s, accessing healthcare services typically involved a physical visit to doctors' offices, clinics, or hospitals, where individuals were identified as "patients."
However, the past decade has witnessed a significant advancement in digital technologies and a shift of the healthcare experience to the digital domain, and the significance of UX in digital healthcare is becoming more apparent.2-6
Simultaneously, the term "patients" has evolved to "healthcare consumers" — a designation suggesting choice and competition. Consumers expect more from the health system than merely having their basic needs fulfilled; they anticipate a superior experience. Despite this, in the realm of healthcare, patients, their caregivers, and healthcare professionals often encounter a user experience that falls short of what they experience in other aspects of their personal lives.7-9
This disparity between what patients expect and what is delivered in terms of the digital patient experience can lead to frustration, a loss of trust, and adversely affect patient care.3,9-11 It is crucial for healthcare providers, health systems, and other organizations to comprehend and align with these patient expectations, and to enhance their digital experiences, thereby boosting patient engagement and satisfaction along their care journey.
The Challenge of Understanding Patients’ Digital Healthcare Needs and Expectations
Despite some research into patient needs and expectations, pinpointing precisely what patients need and expect in the digital world remains a complex task. Up until recently, there were no comprehensive, standardized frameworks or a checklists that summarize these findings or provide an easy-to-use benchmarking tool for patient digital experience. The two prevalent scales for measuring user experience, the System Usability Scale (SUS) and the Net Promoter Score (NPS), are not tailored to healthcare.
The SUS, established in 1986 and largely unchanged since, is a widely used metric for user experience assessment.12 However, it is not healthcare-specific, and it poses broad questions like “I found the system unnecessarily complex” or “I felt very confident using the system,” which may not fully capture healthcare-specific nuances.
The Net Promoter Score, even broader in its approach, asks respondents a single question about their likelihood of recommending a product or service.13 While it gauges overall brand perception, this doesn't necessarily align with the unique aspects of patient experiences in healthcare.
Our use of SUS and NPS in evaluating digital healthcare experiences with patients revealed that these models fall short in measuring several critical elements of a first-rate digital patient experience.
Mapping Patients’ Digital Healthcare Needs and Expectations
In order to bridge this gap between what patients expect from digital healthcare and the experience they typically receive, we conducted user interviews and testing across various therapeutic areas. We then used affinity mapping to categorize patient feedback on their needs and preferences in their digital healthcare experiences.
The affinity mapping is based on the reports of 15 studies that included patient interviews and user testing of digital experiences in healthcare. The studies included a total of 133 patients (age: 20-79 years, 45% male / 55% female), offering a diverse and inclusive perspective on digital healthcare experiences.
Each time a patient articulated a preference or highlighted a pain point during the interview or the testing process, it was assigned to a specific criteria, such as empathy, navigation, ease of use, and others. This categorization allowed us to identify and focus on the most frequently mentioned aspects of the patient experience. During the mapping process, certain categories began to stand out due to their frequent mentions by the patients. We carefully tallied these occurrences, revealing a pattern of patient priorities and challenges within the digital healthcare context.
To further substantiate our findings, we conducted an extensive literature search. This was aimed at validating the categories that had emerged as significant in our study. We sought to ensure that these categories resonated with observations made by other groups and were reflective of broader trends and needs in healthcare UX and digital user experience at large. This rigorous approach allowed us to not only map out but also validate the key elements that define and impact the patient’s digital healthcare journey.
Unveiling Patient Digital Healthcare Needs and Expectations
As a result of the affinity mapping process, 12 key criteria emerged as significant to patients in their digital healthcare experiences.14 These criteria ranged widely, encompassing various aspects of user interaction and satisfaction (Figure 1).
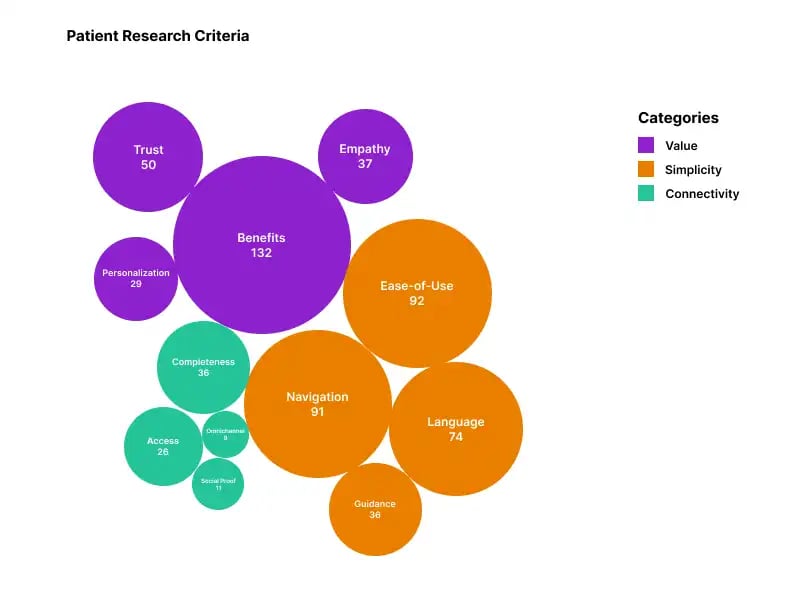
Figure 1. Twelve key criteria emerged as significant to patients in their digital healthcare experience.
Each of these criteria was underscored by varying frequencies of mentions from the patients (Figure 1). This variation in emphasis provided us with valuable insights into how patients prioritize different aspects of their digital healthcare experience. Collectively, these criteria highlight the key themes that are most significant to patients, painting a clear picture of what truly matters to them in their digital healthcare interactions. These criteria also served as the basis for the Patient Experience (PX) Scale — a pioneering framework that uncovers the core principles of patients’ digital expectations and redefines what’s possible in digital healthcare.14
In order to streamline our analysis and make our findings more actionable, we categorized these criteria into logical groupings (Figure 1). This categorization was guided by the nature of each criterion, ensuring that similar or related aspects were grouped together. This approach not only enhanced the clarity of our findings but also facilitated a more structured and focused discussion on how to address these patient preferences and challenges in designing and improving digital healthcare experiences. The criteria were grouped into categories as follows:
- Category 1: Impact:
- Category 2: Simplicity
- Navigation
- Ease of use
- Guidance
- Language
- Category 3: Connectivity:
- Completeness
- Access
- Social proof
- Omnichannel
Validating the Criteria
The literature search suggested that the categories identified through our affinity mapping process were aligned with the findings of other organizations and research groups (Table 1). This consistency confirmed that the themes we unearthed are not isolated observations but are indeed reflective of wider trends and prevalent needs within the broader landscape of healthcare UX and wider digital user experience. This correlation served to reinforce the validity of our findings, indicating that the criteria we identified are representative of the universal needs and preferences in the digital healthcare domain.
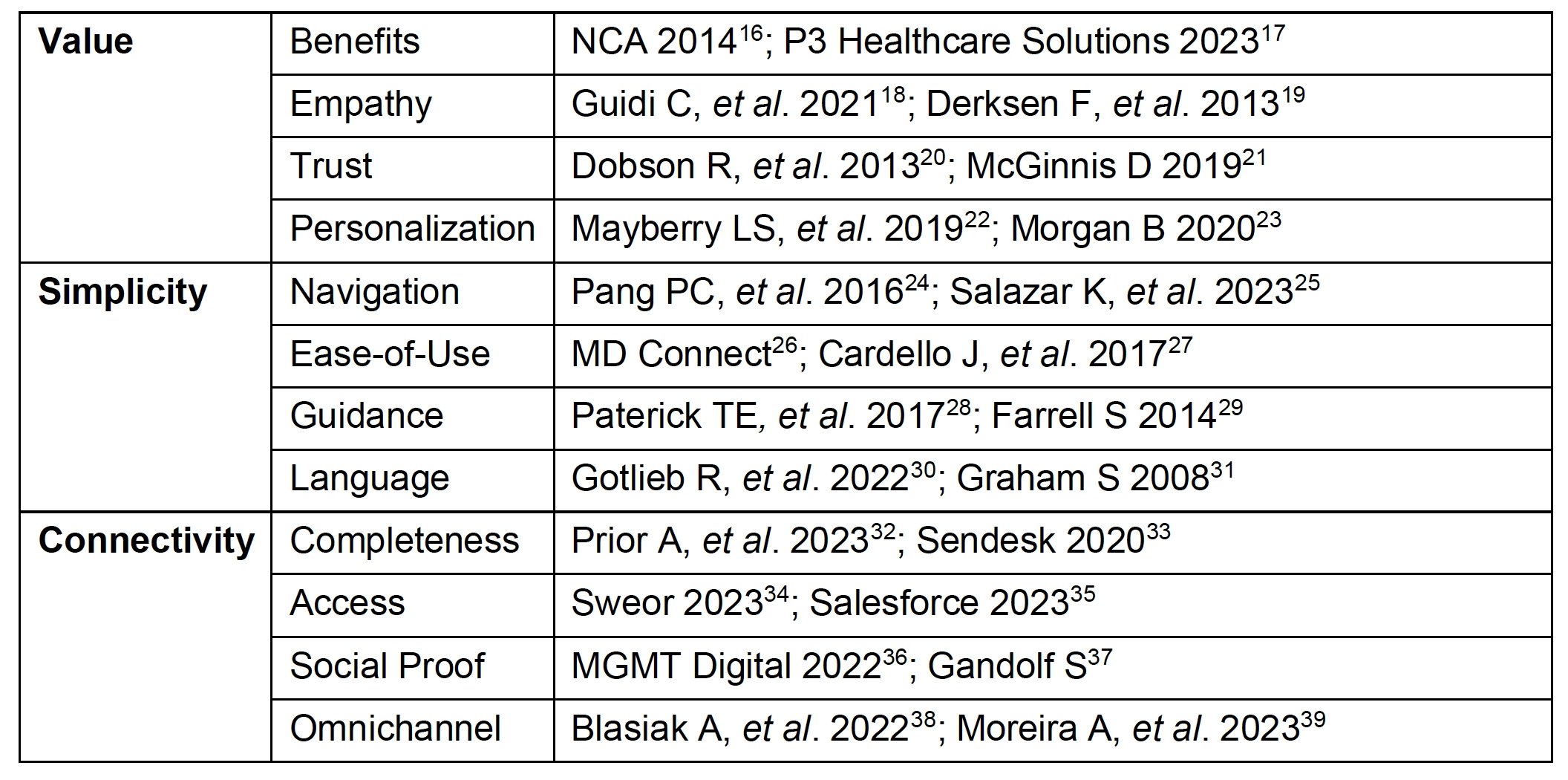 Table 1. Studies validate the criteria identified through the affinity mapping process.
Table 1. Studies validate the criteria identified through the affinity mapping process.
Conclusion
Our research into patient needs and expectations within digital healthcare has been both revealing and validating. The 12 criteria identified through our affinity mapping process represent a comprehensive spectrum of patient priorities, from the value-driven aspects like empathy and personalization to the practicalities of navigation and accessibility. These criteria not only reflect the patients' direct feedback but also align with broader trends observed in healthcare and UX in general.
The convergence of our study's results with existing literature further validates our approach and findings. It highlights the universal nature of these patient preferences, transcending individual experiences to reflect a collective demand for more intuitive, empathetic, and accessible digital healthcare solutions.
Our findings underscore the importance of a user-centric approach in digital healthcare and patient engagement technologies, emphasizing the need for systems that are not only functional but also resonate on a personal and emotional level with patients. As the healthcare industry continues to evolve, these insights provide a crucial roadmap for healthcare organizations. By prioritizing and addressing these key areas, they can enhance patient satisfaction, foster deeper trust, and ultimately lead to higher engagement with medical services and better patient outcomes.
References
1. Knickman JR, Elbel B. Jonas and Kovner's Health Care Delivery in the United States. 13th ed. Springer Publishing Company, 2023.
2. Madanian S, Nakarada-Kordic I, Reay S, et al. Patients' perspectives on digital health tools. PEC Innov. 2023; 2: 100171.
3. Leonardsen A-CL, Hardeland C, Ann Karin H, et al. Patient experiences with technology enabled care across healthcare settings - a systematic review. BMC Health Serv Res. 2020; 20: 1-17.
4. Risling T, Martinez J, Young J, et al. Evaluating patient empowerment in association with eHealth technology: scoping review. J Med Internet Res. 2017; 19.
5. Akbar A, Iqbal A, Gaziano D, et al. A cross-sectional survey on telemedicine use for doctor-patient communication. Cureus. 2020; 12.
6. Sheridan NF, Kenealy TW, Fitzgerald AC, et al. How does it feel to be a problem? Patients' experiences of self-management support in New Zealand and Canada. Health Expect. 2019; 22: 34-45.
7. Why don't patients love pharma apps? Because most are just mediocre, advocacy network says. Fierce Pharma. https://www.fiercepharma.com/marketing/patients-lackluster-interest-pharma-apps-tied-to-low-awareness-and-value-says-patient. Date accessed: January 24, 2024.
8. Gilbert RM. Reimagining digital healthcare with a patient-centric approach: The role of user experience (UX) research. Front Digit Health. 2022; 4: 899976.
9. Birnbaum F, Lewis DM, Rosen R, et al. Patient engagement and the design of digital health. Acad Emerg Med. 2015; 22(6): 754-756.
10. Marks R, Allengrante JP, Lorig K. A review and synthesis of research evidence for self-efficacy-enhancing interventions for reducing chronic disability: implications for health education practice (part I). Health Promot Pract. 2005; 6(1): 37-43.
11. Hibbard JH, Mahoney ER, Stock R, et al. Do increases in patient activation result in improved self-management behaviors? Health Serv Res. 2007; 42(4): 1443-63.
12. System Usability Scale (SUS). Usability.gov. https://www.usability.gov/how-to-and-tools/methods/system-usability-scale.html. Date accessed: January 24, 2024.
13. What Is Net Promoter? Net Promoter Network. https://www.netpromoter.com. Date accessed: January 24, 2024.
14. Patient Experience (PX) Scale. Intechnic. https://www.intechnic.com/pxs. Date accessed: October 29, 2024.
15. Why you only need to test with 5 users. NN/g Nielsen Norman Group. https://www.nngroup.com/articles/why-you-only-need-to-test-with-5-users. Date accessed: January 24, 2024.
16. Patients Are Signing Consent Forms They Don’t Understand. We Can Do Better. National Communication Association. 2014. https://www.natcom.org/communication-currents/patients-are-signing-consent-forms-they-don%E2%80%99t-understand-we-can-do-better. Date accessed: January 24, 2024.
17. What is a Value Proposition in Healthcare? P3 Healthcare Solutions. 2023. https://medium.com/@outsourcemedicalbilling1/what-is-a-value-proposition-in-healthcare-70b1fefabc3d. Date accessed: January 24, 2024.
18. Guidi C, Traversa C. Empathy in patient care: from ‘Clinical Empathy’ to ‘Empathic Concern’. Med Health Care Philos. 2021 Dec;24(4):573-585.
19. Derksen F, Bensing J, Lagro-Janssen A. Effectiveness of empathy in general practice: a systematic review. Br J Gen Pract. 2013;63(606):e76-84.
20. Dobson R, Wihongi H, Whittaker R. Exploring patient perspectives on the secondary use of their personal health information: an interview study. BMC Med Inform Decis Mak. 2023 11;23(1):66.
21. McGinnis D. 40 Customer Service Statistics To Move Your Business Forward. Salesforce. 2019. https://www.salesforce.com/blog/customer-service-stats. Date accessed: January 24, 2024.
22. Mayberry LS, Nelson LA, Greevy RA, et al. 819-P: Personalized Texts Improve Adherence and A1c over 6 Months among High-Risk Adults with Type 2 Diabetes. Diabetes. 2019;68(Supp 1):819-P.
23. Morgan B. 50 Stats Showing the Power Of Personalization. Forbes. 2020. https://www.forbes.com/sites/blakemorgan/2020/02/18/50-stats-showing-the-power-of-personalization. Date accessed: January 24, 2024.
24. Pang PC, Chang S, Verspoor K, et al. Designing Health Websites Based on Users' Web-Based Information-Seeking Behaviors: A Mixed-Method Observational Study. J Med Internet Res. 2016 Jun 6;18(6):e145.
25. Salazar K, Katsarakes A. Digital Interactions in Healthcare Customer Journeys. Nielsen Norman Group. 2023. https://www.nngroup.com/articles/healthcare-customer-journeys. Date accessed: January 24, 2024.
26. For Medical Websites, User Experience Can Matter Even More than Patient Trust. MD Connect. https://www.mdconnectinc.com/medical-marketing-insights/medical-marketing-insights/medical-websites-user-experience. Date accessed: January 24, 2024.
27. Cardello J, Farrell S. HealthCare.gov’s Account Setup: 10 Broken Usability Guidelines. Nielsen Norman Group. 2017. https://www.nngroup.com/articles/affordable_care_act_usability_issues. Date accessed: January 24, 2024.
28. Paterick TE, Patel N, Tajik AJ. Improving health outcomes through patient education and partnerships with patients. Proc Bayl Univ Med Cent. 2017; 30(1): 112-113.
29. Farrell S. FAQs Still Deliver Great Value. Nielsen Norman Group. 2014. https://www.nngroup.com/articles/faqs-deliver-value. Date accessed: January 24, 2024.
30. Gotlieb R, Praska C, Hendrickson MA, et al. Accuracy in Patient Understanding of Common Medical Phrases. JAMA Netw Open. 2022;5(11):e2242972.
31. Graham S, Brookey J. Do Patients Understand? Perm J. 2008;12(3):67-69.
32. Prior A, Vestergaard CH, Vedsted P, et al. Healthcare fragmentation, multimorbidity, potentially inappropriate medication, and mortality: a Danish nationwide cohort study. BMC Medicine. 2023;21:305.
33. Zendesk Customer Experience Trends Report. Zendesk. 2020. https://d1eipm3vz40hy0.cloudfront.net/pdf/cxtrends/cx-trends-2020-full-report.pdf. Date accessed: January 24, 2024.
34. Eye-Opening Website Statistics: Is Your Website Costing You Clients? SWEOR. 2023. https://www.sweor.com/firstimpressions. Date accessed: January 24, 2024.
35. The Fifth Edition State of Service Report. Salesforce. 2023. https://www.salesforce.com/resources/research-reports/state-of-service. Date accessed: January 24, 2024.
36. Why Is Social Proof Important on Healthcare Websites? MGMT Digital. 2022. https://mgmtdigital.com/why-is-social-proof-important-on-healthcare-websites. Date accessed: January 24, 2024.
37. Gandolf S. 6 Ways to Influence and Persuade with Social Proof. Healthcare Success. https://healthcaresuccess.com/blog/advertising/6-ways-to-influence-and-persuade-with-social-proof.html. Date accessed: January 24, 2024.
38. Blasiak A, Sapanel Y, Leitman D, et al. Omnichannel Communication to Boost Patient Engagement and Behavioral Change With Digital Health Interventions. J Med Internet Res. 2022;24(11):e41463.
39. Moreira A, Alves C, Machado J, et al. An Overview of Omnichannel Interaction in Health Care Services. Mayo Clin Proc Digit Health. 2023;1(2):77-93.


